Julian Assange
636 weeks of deprivation of liberty for telling the truth
636 weeks of deprivation of liberty for telling the truth
The numbers, compiled by Sciensano, relayed unfiltered by the media and used by our government for political purposes, make our heads spin daily. Annès Bouria gives us however in a weekly way a very different interpretation.
This analysis is based on the Sciensano epidemiological report dated 31/10/2020. [1]
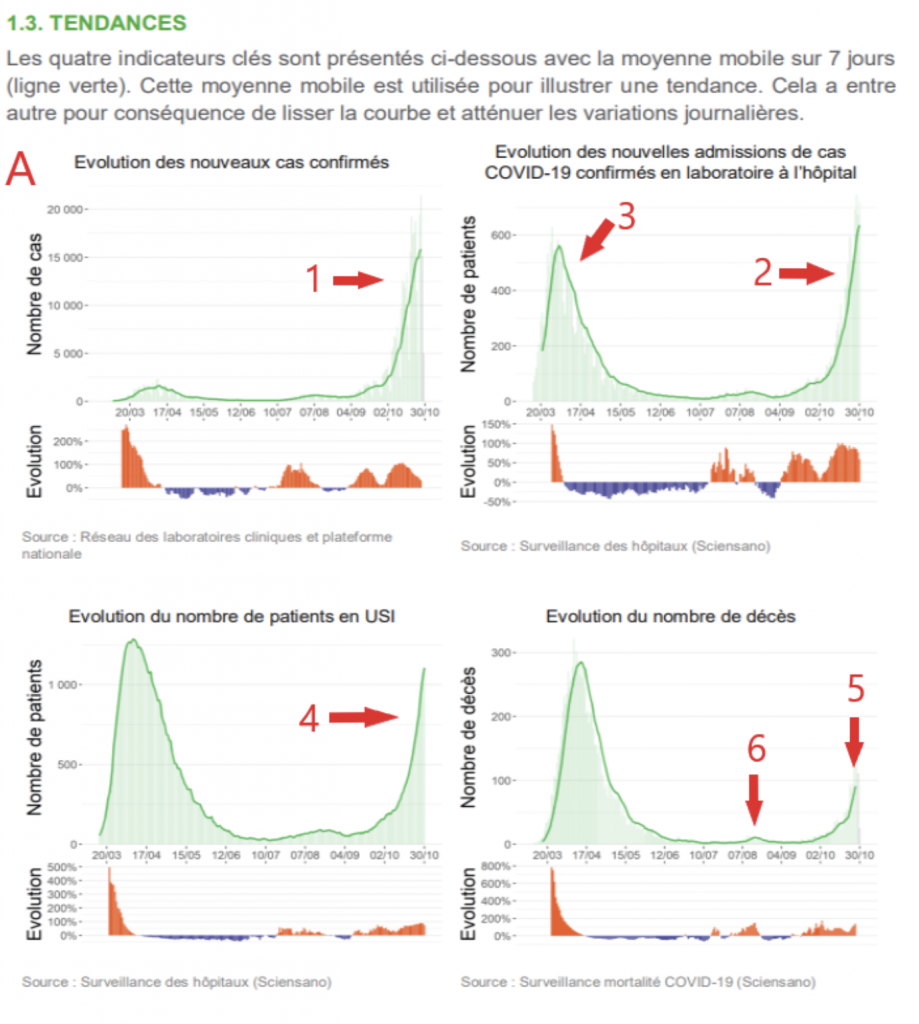
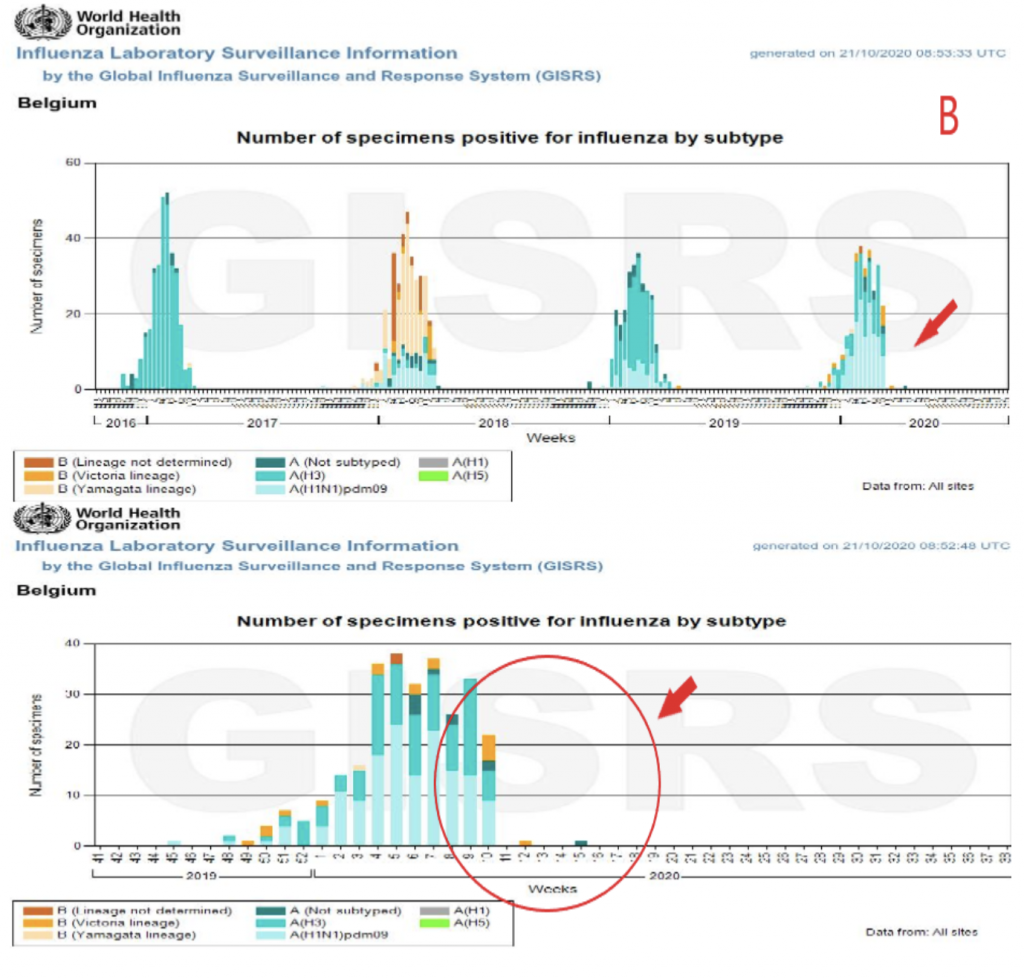
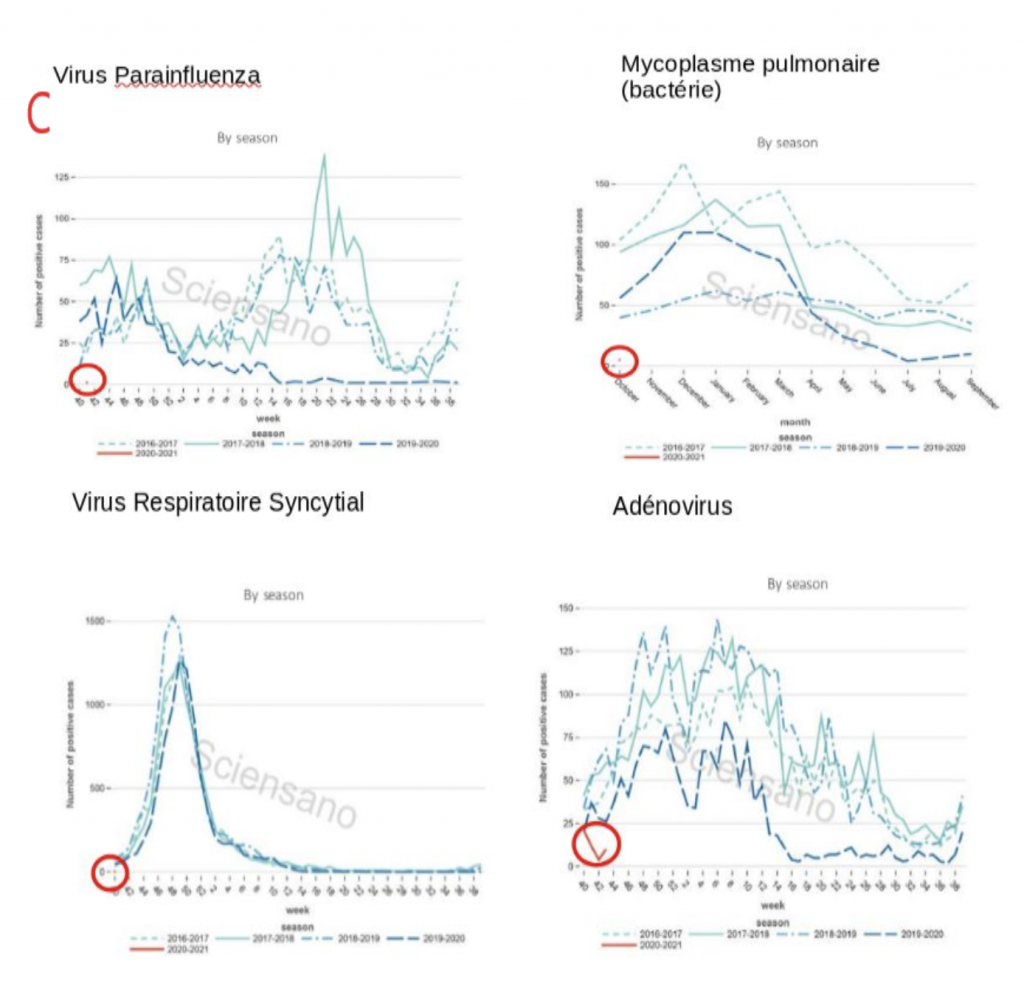
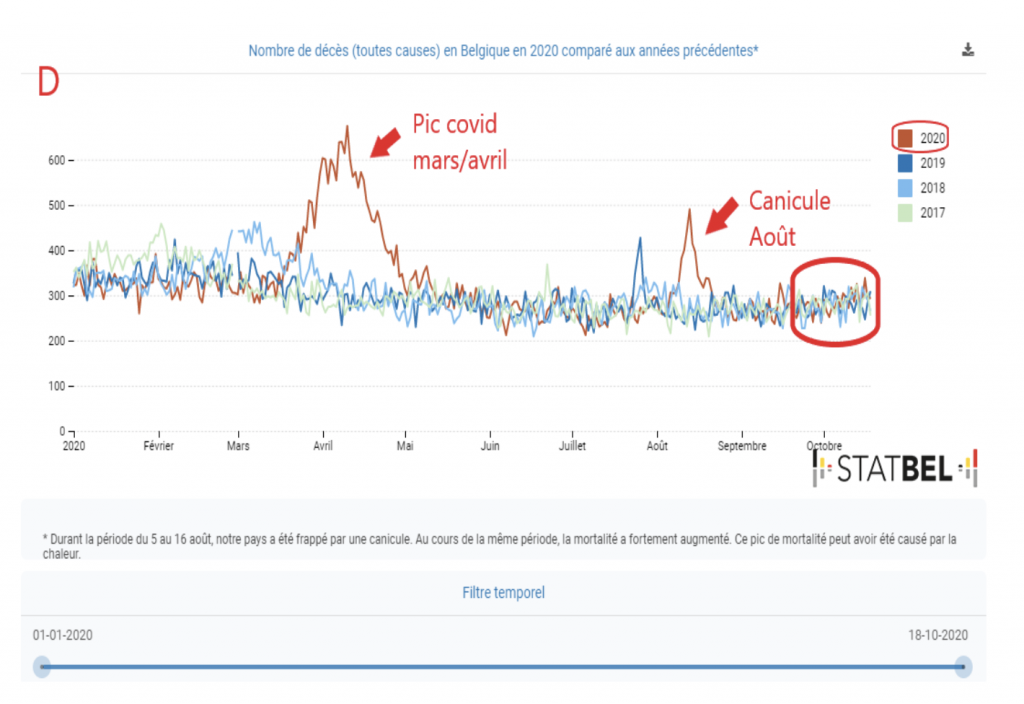
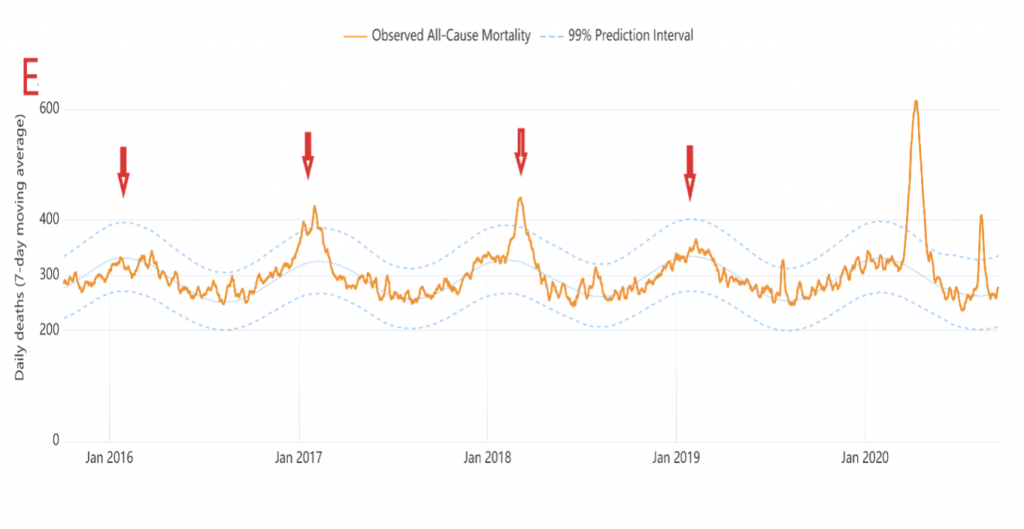
Below we have in A, the epidemiological graphs of covid published by Sciensano, in order: 1 the number of cases, 2 and 3 hospitalizations, 4 patients in intensive care, 5 and 6 mortality. In B, the WHO epidemiological graphs of influenza cases in Belgium [2]. In C, the epidemiological graphs of the census of cases of various seasonal respiratory pathogens from Sciensano and published by Christophe de Brouwer, Professor at the School of Public Health of the ULB. In D A graph of overall mortality data from 2016 to 2020 compiled by Statbel [3]. And finally in E, the graph of mortality over time in Belgium from 2016 to 2019 from the Belgian Mortality Monitoring [4]
1. There continues to be a highly significant increase in the number of positive tests to an average of 15850 per day per week. It is always good to remember that these are not always « cases » in the clinical sense of the term and that the majority have benign forms of the disease.
To know the proportion of cases considered serious, the index consists in dividing the average number of daily admissions of 640 patients by the 15850 positives, which makes 4% of the positives requiring hospitalization. A very slight increase in numbers may be due to the new guideline of no longer testing asymptomatic patients.
It should also be remembered that this peak of positives is not at all comparable to the one in March-April when only patients who arrived at the hospital in very advanced stages were tested. Today the testing policy is still very broad, more than 450,000 tests were performed the previous week. The number of PCR tests is close to 80,000 per day, almost one and a half million tests were performed in one month! This is akin to a massive testing campaign. The recent decision to stop testing asymptomatic patients is welcome. Indeed, since this summer, the testing policy was not targeted and most of the healthy carriers whose contagiousness is not established were detected [5].
2. As for the increase in hospitalizations classified as « covid », they are rising exponentially.
Nevertheless, here are some theoretical but factual figures: covid patients occupy about 6500 beds, i.e. about 18% of all available clinic beds in the whole territory (37 000) or 81% of the 8000 beds potentially available for covid cases [6]. The 650 average daily hospitalizations classified as « covid » for the week of October 25–31 represent less than 54% of the approximately 1200 daily hospital contacts for respiratory complaints according to 2017 data from FPS Public Health [7]. For an average of 650 admissions per day, approximately 450 discharges are recorded.
It should also be noted that the distribution of hospitalizations is not homogeneous: the Brussels Capital Region, the provinces of Hainaut and Liège alone account for almost half of the new admissions.
The imminent threat exposed by experts as well as political authorities is that of hospital saturation. Although the situation is indeed very tense, the phenomenon of hospital saturation during periods of increased seasonal illnesses is unfortunately not new, there were episodes of winter saturation in 2017 as well as in 2019 during the influenza epidemics [8,9]. If we want to probe the reasons for this chronic saturation of hospitals, it is important to take into account the clear decrease of available beds for acute conditions in hospitals over the last 30 years, from more than 55,000 to 37,000, despite the increase of the population and its aging! [7]
It would also be interesting to question the authorities to know what they have concretely put in place in terms of hospital resources to deal with the situation that they have been dreading for more than 6 months. Especially since some sources mention a problematic rate of absenteeism among health care personnel attributable to the management of the health crisis as well as to the consequences of the latter: illnesses (burn out?), quarantines, parental leave corona, taking of accumulated vacation days or recovery days for overtime worked… [10] It is important to question the public authorities about this situation: was it not foreseeable? It is difficult to control epidemic dynamics, but isn’t managing human resources in a hospital setting within the public sector not only possible, but also within your prerogatives and responsibilities?
Especially since the situation in hospitals and even in outpatient clinics is heavily burdened by « covid » protocols, not only in terms of clinical management but also at the administrative level, preventing medical staff from concentrating on their primary function, which is to provide care. Are these protocols, which place a huge burden on hospital staff and primary care physicians, common sense and absolutely necessary [11,12,13]?
Finally, the most important point, in my opinion, is that there is absolutely no policy for outpatient treatment of patients with covid. In this epidemic, general practitioners who are supposed to be on the front line are out of the running. According to official recommendations, they have only one course of action to follow for symptomatic positive cases: isolation, paracetamol and, in extremis, referral to a hospital if the patient’s condition deteriorates [14]. In the history of medicine, this is unheard of! Wouldn’t this policy of not taking care of patients be, among other things, the reason for the over-occupation of covid hospitals?
3. We are likely to face a new epidemic episode of covid. However, apart from the obvious hospital tensions, is this episode on the same scale as the first? A priori, the current curve seems to exceed the one of March, but it is necessary to take into account that the appearance of seasonal respiratory diseases (autumn-winter) makes that there are more suspicions of clinical cases covid, that the PCR tests, whose sensitivity is very high and the specificity not absolute, will not always be able to distinguish from the other seasonal respiratory viruses This is the problem of false positives. [15] I would like to emphasize that these are false positives in the diagnostic sense of the term and not in the technical sense. The test does detect a trace of the virus, but this does not give us any clear information about the etiology of the patient’s clinical condition.
The difficulty lies in clearly distinguishing seasonal respiratory diseases from covid, which is not possible to establish with any certainty.
Are all patients admitted and listed as « covid » sick because of SARS-COV2 infection, or are they suffering from other respiratory infections while carrying SARS-COV2 without SARS-COV2 being the major cause of their clinical condition? [16]
On this important point, I refer you to the charts B C:
On the graphs B: the first one shows the changes of the influenza virus at each seasonal peak of influenza in Belgium since 2016. The second one concerns only the last influenza season, and we see that the peak stops abruptly at the 10th week, from March 2 to 8. This is an intriguing anomaly that corresponds very closely to the week of the start of the sars-cov‑2 epidemic in our country in late winter. The only coherent explanation according to Christophe de Brouwer, Professor at the School of Public Health of the ULB, would be that influenza, at the end of the epidemic peak, would have been taken for covid! What is the situation today? Are we strictly distinguishing between covid and other seasonal respiratory infections?
On the C charts: these represent the epidemic curves of various seasonal respiratory pathogens. Apart from an early resurgence of influenza A (often confused with covid) 4 other seasonal respiratory diseases have literally disappeared from the radar. Could this rather unusual anomaly suggest that a certain proportion of patients labeled « covid » are in fact suffering from other conditions while being PCR positive or are listed as « covid » simply as a precautionary measure?
It is important to note that according to some studies, depending on the sensitivity of PCR tests, up to 90% of positive tests for SARS-COV2 have no medical significance when systematized to this extent. Indeed, a New York Times article reports this very high proportion of clinically irrelevant positives when the number of PCR amplification cycles (CT) exceeds 30 [17]. And in Belgium, the number of PCR amplification cycles (CT) ranges from 30 to 35 [15].
If the CT cycles of the PCRs performed are too high, the tests are hypersensitive and therefore cannot determine, even if positive, whether the patient is indeed sick with covid.
All these patients labelled « covid », whether they really have this disease or not, will in fact cause a rapid saturation of the hospital system because of the cumbersome protocol of their care.
Add to that the fact that some patients admitted for anything other than covid are tested for PCR, and if they are positive, they are listed as « covid hospital admissions »!
4. The number of intensive care unit (ICU) patients also exponentially tracks hospitalizations. There are 1,150 ICU patients nationwide. This is 57% of the critical care bed capacity (approximately 2000) [18].
As for the saturation of the intensive care units in Belgium, unfortunately this is not an exceptional situation either. According to Dr. Philippe Devos, intensivist at the CHC Liège, during the peak of the flu epidemic in January/February 2020, the ICU bed occupancy rate was over 90%! And this by patients who developed complications from severe influenza [19].
ICU capacity is well stretched by the cases listed covid. But what is imperative to highlight is that the clinical covid pictures are much less gloomy than in March/April. The proportion of ventilated patients has decreased since the last episode in March, and it is indeed the patients on ventilators who have the worst vital prognosis and who « clog up » the ICUs because their management is spread over several weeks, which reduces the « turn-over » capacity of the resuscitation passages. Indeed, this improvement in terms of « severity » of cases may be due to a mutation of the virus to a less lethal form, or to better management of patients upstream thanks to a better knowledge of the disease as well as to the introduction of treatments such as anti-coagulants, corticosteroids or oxygen therapy which reduce ICU visits and their severity. [20]
It is clear that management protocols have changed and that intubations are only done as a last resort. This highly invasive medical technique constituted more than 80% of the management of covid patients in the ICU during the April epidemic peak, compared to about 50% today. And this is confirmed by a lower covid mortality at the present time.
5. The « covid » mortality increases significantly: 91 deaths per day on average for the whole of Belgium. As a reminder, there are nearly 300 deaths per day on average in Belgium for all causes combined, and this figure can rise to 400 in the winter period. In « instantaneous » lethality rate we are at 0.57%. This figure has increased slightly, also due to the fact that asymptomatic patients are no longer tested. There were nearly 300 deaths per day at the peak of mortality in April. Mortality is currently 3 times lower than during the previous peak.
Fortunately, there was less of an increase in mortality compared to the other indicators, which is a major indication that this episode was less severe than the March/April peak. So I would refer you to Graph D which is the general mortality data, there is, through October 18, no excess general mortality over the previous three years with respect to this fall 2020 epidemic episode. The mortality will undoubtedly stand out in the next few weeks, but one can hope that it will be out of proportion to the March/April peak.
6. The small peak of mortality in 6 is due to the heat wave of August (see graph B as well), but still appears on the graph of covid mortality, proof that the label « covid » in terms of mortality, and a fortiori of clinical cases, is not always rigorously reliable.
To support this fact I quote the note regarding deaths on page 17 of the Sciensano epidemiological report: « Since May 5, 2020, deaths of possible cases in hospital are also taken into account. Deaths of possible cases refer to patients who did not have a diagnostic test for COVID-19, but who met the clinical criteria for the disease according to the physician. Out-of-hospital deaths (nursing homes, other residential communities, home, other locations) are reported by regional authorities and represent deaths of confirmed and possible cases. »
It should also be noted that each year mortality increases in winter, particularly due to seasonal infections (influenza, among others). This is best illustrated in graph D.
Are the increases in covid mortality, let alone hospitalizations, attributable only to this disease, given the difficulty of differential diagnosis between covid and other respiratory infections? [21]
*Averages for the week of 10/25 to 10/31
In conclusion, we can now note very highly significant increases in hospitalizations catching up with the levels of the March/April episode. Nevertheless, the situation is not comparable to the spring peak in terms of the rather favorable clinical pictures and the lethality which remains relatively low.
It seems very likely that SARS-Cov2 is taking on a seasonal pattern and that this virus, which until now has been circulating at a low level like many endemic viruses, is peaking in the early fall. Isn’t this one highlighted in an exaggerated way by an excessive focus around it? If we tracked other endemic viruses such as influenza A or RSV with the same obsession, would we not have more or less the same epidemiological indicator values? Or better yet, wouldn’t we actually be on the verge of reaching a threshold of collective immunity? In which case, the government’s actions would be the exact opposite of what should be done. [22]
In any case, it is clear that the measures taken over the past month to change the indicators have been totally ineffective. In an ill-considered headlong rush by our government, supported by a unanimous and dogmatic expertocracy, we are once again subjected to a strategy of containment that is highly questionable on all levels, medical, socio-economic and constitutional.
It should be remembered that, firstly, the effectiveness of containment has not been demonstrated. The countries that have applied this measure drastically are among those with the most catastrophic per capita mortality rates in Europe: Belgium, Spain, Italy, the United Kingdom and France. Add to this the fact that a seroprevalence study conducted by the Spanish authorities on more than 60,000 subjects concluded that confined persons were more contaminated than persons who continued their professional activities in the essential sectors. Data confirmed by another Italian study that can legitimately cast doubt on the strategy of containment as a solution to the epidemic. [23,24]
And secondly, the collateral damage in terms of health of such a strategy seems to tip the balance in favor of the risks rather than the benefits. As shown by several British studies which highlight an unprecedented increase in late diagnosed cancers and heavy consequences on untreated pathologies such as cardiovascular accidents. Not to mention suicides, depression and the resurgence of intra-family violence [25].
Why didn’t you measure the effects of this totally unprecedented, even medieval, strategy before rushing headlong into renewing it?
Furthermore, the much feared phenomenon of saturation of public hospitals seems to be very much attributable to the chronic lack of hospital resources. If this is the pitfall to be avoided, it seems very risky to persist in the crescendo of coercive measures that, empirically, do not seem to be effective. These unconstitutional measures are, moreover, coupled with a dialectic consisting solely of making the citizen feel guilty, by imposing these restrictive measures without questioning the responsibility of the authorities. This is clearly an extremely disingenuous and dishonest political strategy in terms of transparency about the complexities of the ins and outs of this health crisis.
A well thought-out strategy with regard to the risk/benefit balance (not only from a health point of view, but also from an economic and social point of view) would be to put general practitioners back on the front line. The prerequisite and sine quo non is to lighten their administrative protocol loads in order to allow them autonomy in the management of covid patients in the outpatient setting. This means directing prophylaxis to those at risk and reserving testing and hospitalization only for those cases where it is deemed necessary by the treating physician. The latter are equally capable of treating moderately severe forms with combinations of antibiotics (azithromycin/cefuroxime), prescribing Plaquenil® if they so choose, administering corticosteroids and anticoagulants as a preventive measure, and even resorting to home oxygen therapy for more advanced forms. All of this under a close and attentive supervision.
Finally, the most important remarks: is the increase in hospitalizations classified as « covid » « drowned » in a normal phenomenon of recrudescence of winter respiratory diseases for which a differential diagnosis with covid is not absolutely determinable? At what intensity does Sars-Cov2 really circulate? Is its current form as lethal as last spring? Are we dealing with an epidemic episode of the same magnitude as the first one or is it the highlighting of a seasonal peak of the virus by a massive testing policy?
These questions deserve in-depth investigations as their implications are so important for the daily life of citizens.
Thank you for reading.
Annès Bouria
Pharmacist — Member of the Transparency-Coronavirus collective
https://www.transparence-coronavirus.be/