
Julian Assange
631 weeks of deprivation of liberty for telling the truth
631 weeks of deprivation of liberty for telling the truth
By
The Covid crisis has followed, quite globally but especially in the West, a similar orientation in its decisional management:
It is in France that a debate has crystallized that could be called epistemic (or epistemological). That is to say, it questions the very mode of learning and practicing medicine, between, on the one hand, the protagonists of a hegemonic EBM who act solely on the basis of proof of the effectiveness of a treatment. This evidence must be based on a randomized controlled trial and peer review. On the other hand, we find the protagonists of a medical practice where EBM accompanies clinical experience and intervenes as a tool to help decision-making, but does not prevent it in favor of individual responsibility.
This opposition has sometimes been relayed in the press as that between « scientists and empiricists »(1). If this is the right way to put it, there is the risk of considering scientific knowledge as being only on the side of the « scientists », hence the violent and socially prejudicial « boycott » of those who are called « charlatans », for example.
However, this is to misunderstand the original definition of EBM. Indeed, if we refer to authors like Sackett(2)The objective of EBM was to propose a new framework to guide medical action, judiciously articulating the experience of practitioners, the best available scientific data (at a time « T0 » appropriate for action ’ ), and the best available information.hic and nunc’), and the preferences of an informed patient, in line with the clarification developed by Folscheid(3)According to this statement, despite the widespread stereotype that medicine has changed from an art to a science, » medicine is […] neither a science nor a technique, but [bien] a personalized care practice, accompanied by science and instrumented by technical means « that is, a praxis.
The problem is that the original EBM project has radically narrowed as a result of a techno-scientific and normative drift(4) as insidious as it is implacable, on a positivist conception of demonstration and proof. The latter is probably perceived as the only source of reassurance in the face of the uncertainties to be faced.
This need for certainty leads us to exonerate ourselves from our individual responsibility in making decisions by delegating them to science or technology. Thus, the practitioner’s experience, the relational and always singular dimension with his patient, and the eminently specific context on many levels are lost. Everything that makes the diversity of the individual. On the other hand, by delegating our doubt to the method alone (experimental in the case of EBM), we give full credit to a positivist science that can, today more than ever, be deviated(5). An example of this was the scandal of the Lancet article(6).
In medical education, the dominant, even hegemonic, institutional epistemology is positivist. That is to say that medical knowledge will be acquired primarily through long years of study, based on knowledge deemed universal on the basis of the positivist scientific method.
However, by following this path, we realize that we are losing two essential elements, which have, moreover, been greatly missed in the management of this crisis:
1) An epistemology that is closer to the field, to situations, to action, in other words, an epistemology of experience, of process or of action(7) rather than of knowledge or theory alone, of figures and statistics that are intended to be universal;
2) An epistemology that is more open and not reduced (reductionist) to the positivist method alone, i.e. an epistemology that favors science in the plural, in reference to the work of Leo Coutellec(8)
Another way to approach this problem is to start from these figures. If the critical mass of medical students is trained primarily on the basis of an accumulation of theoretical knowledge defined by the positivist method, it will be difficult for them, in their professional practice, to break away from a safe need for protocols, standards, guidelines and EBM(9). Covid 19 illustrated this problem.
Figure 1(10) below proposes a critical look at medical training curricula where the challenge would be, on the contrary, to start from the capabilities expected in real life, and to bring ‘all this uncertainty’ into the training curricula. This is what is developed in the referenced forum.(11)
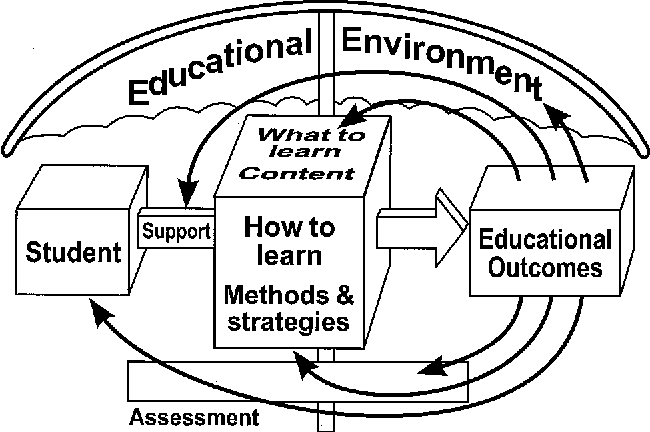
Starting from reality (from lived professional situations) in order to build a curriculum would then allow the development of professional skills in recognition of knowledge coming from epistemologies of other disciplinary fields (12). Such an attitude opens up interprofessionality(13), emotional and relational intelligence (14), as well as attention to ethical issues such as prejudices and discriminatory phenomena easily conveyed in the very standardized environment of the medical world (15), but also those related to patient autonomy(16).
We have seen this with the decisions, or positions, regarding non-therapeutic interventions and prophylaxis, all of which are so at odds with the WHO definition of health: » Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity. The holistic vision of the person was totally lacking, reflecting very directly the orientation of medical training: bioclinical, EBM, normative and hospitalocentric.
Figure 2 below shows how pedagogy is a « lever » that contributed to the hospital-centric management of the Covid 19 crisis. We quote from an editorial published in a medical education journal(17), reproducing in full an excerpt from the commentary that accompanied it. This is thanks to Charles Boelen, coordinator of the dictionary on the social responsibility of medical schools(18):
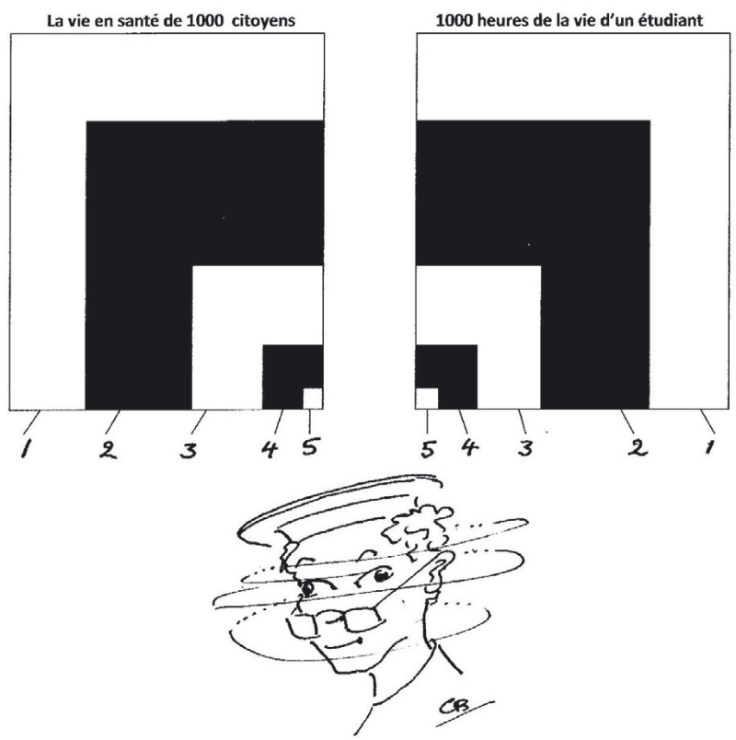
Out of a population of 1000 citizens (see area 1 in the table on the left), 750 will present with a health concern (area 2), of which 250 will consult a primary health care provider (area 3). Of these, 50 will be reviewed by a specialist (area 4) and one (area 5) will be admitted to the university hospital. The chart on the right parallels 1000 hours of a medical student’s practical training. It should be noted that a large part of his time is spent in hospitals (area 1), with a propensity for specialized services (area 2), much less frequentation of peripheral hospitals or health centers (area 3), a few hours in general practice (area 4), and a few hours in the hospital (area 5). 4) and very little time in settings that allow them to understand the determinants of health in the general population (area 5). Let’s compare the two tables: the hourly volume of practical training seems inversely proportional to the epidemiology and frequency of situations to which citizens are exposed.
We are not surprised by this discrepancy! Even today, most of the functions attributed to the physician relate to disease control, leaving less room for health strategies and their corollaries of prevention, education and promotion.
- EBM is a decision support tool and should not replace the responsibility of the decision maker(s);
- Medicine is a praxis currently based on an epistemology of science and not of action, generating a situation that is the source of many ambiguities experienced during the crisis of the Covid;
- Medical training does not prepare physicians for a global vision of the health system, the individual, or health itself;
- In medical training, the priority given to decisive judgment(19) over reflective judgment determines the medical world as a breeding ground for normative drift.
These elements have strongly contributed to the orientations of the management of the health crisis.
We encourage the reader to extend this reflection by referring to the forum: Becoming a Physician Tolerating Uncertainty — The Next Medical Revolution?(20) whose last sentence concludes our carte blanche:
« Ironically, only un-certainty is a sure thing. Certainty is an illusion ».