Dès la fin de l’été 2020, les médias de différents pays relayaient la crainte d’une « double épidémie » coronavirus et grippe, les experts insistant sur l’importance de la vaccination contre la grippe(1). En effet, le New York Times informait notamment que le Centers for Disease Control and Prevention (l’agence fédérale de la santé publique des Etats-Unis) avait commandé 9,3 millions de doses supplémentaires aux 500.000 doses annuelles de vaccins contre la grippe en 2020(2). Si l’inquiétude généralisée d’une double épidémie, portant le néologisme de « twindemic », s’est estompée avec l’absence totale de la grippe pendant la pandémie du COVID-19 (non seulement en Belgique et en Europe, mais partout dans le monde(3), la sonnette d’alarme a été tirée à nouveau en cette début d’année 2022. Effectivement, l’agence de presse Reuters a annoncé le retour de la grippe qui pourrait menacer l’Union Européenne selon les experts du Centre Européen de Prévention et de Contrôle des Maladies (ECDC), entraînant une épidémie prolongée avec le SARS-CoV‑2, ce qui résulterait, on pouvait le deviner, en une pression dangereuse sur notre système de soins de santé(4). Avec 650.000 morts annuels attribués à la grippe dans le monde (dont 72.000 en Europe)(5), les effets synergiques avec l’épidémie du coronavirus à craindre seraient de deux natures:
- Une mortalité plus élevée liée à une co-infection coronavirus + grippe, ainsi qu’à la nature virulente de la souche de la grippe (H3 de la Grippe A)(6) (7)
- Un décalage de la période grippale saisonnière entraînant un prolongement inhabituel de la circulation du virus de la grippe au-delà du printemps et un allongement des épidémies respiratoires(8)
L’énoncé de la peur d’une « twindemic » est donc accompagné par un appel à la vaccination ainsi que par le maintien implicite des mesures sanitaires(9). Rappelons que l’efficacité des vaccins contre la grippe, estimée à environ 30–60% selon les années(10), est surtout basée sur la capacité de prédiction de la souche virale qui arrivera sur notre territoire, déduite en fonction des observations effectuées dans d’autres pays. De fait, il serait actuellement très difficile d’élaborer ces vaccins, car la grippe a été absente pendant la pandémie. Malgré cela, cela n’empêcherait pas les autorités sanitaires d’inviter la population à se faire vacciner contre la grippe, tout en respectant les mesures sanitaires pour une protection plus solide.
Mais qu’en est-il de la science derrière l’appréhension d’un double épidémie?
Comme bien souvent, il y a des éléments de vérité dans les énoncés à partir desquels sont ensuite extrapolés des prédictions apocalyptiques (Neil Ferguson, épidémiologiste de l’Imperial College en Angleterre, est un spécialiste de ce domaine sinistre et est responsable, de par ses modélisations, entre autres des lockdown de la pandémie actuelle(11). Il convient toutefois d’accorder qu’effectivement il est tout à fait possible de contracter simultanément le COVID-19 et la grippe(12), tout comme il est possible d’être co-infecté par le SARS-CoV‑2 et un autre virus respiratoire (des cas cliniques en début 2020 ont été documentés sur ces infections multiples)(13). Seulement, ces données sont à mettre dans leur contexte en prenant plusieurs facteurs en compte:
- L’épidémiologie des co-infections virales (des maladies respiratoires) est un domaine peu étudié(14)
- Les données disponibles ne permettent pas de conclure sur la dangerosité des maladies causées par ces infections multiples, plusieurs études n’observant pas de différence de mortalité et/ou morbidité entre ces dernières et les infections simples(15)
- Le phénomène « d’interférence virale » pourrait avoir l’effet inverse: un virus pourrait en écarter un autre
Le concept de l’interférence virale est le suivant: les virus provoquant des symptômes similaires peuvent se retrouver en compétition l’un avec l’autre, ce qui entraîne l’exclusion d’un ou plusieurs virus par un virus dominant. En biologie, ce type de phénomène a été bien décrit et théorisé dans le concept de la « niche écologique ». Selon ce dernier, les organismes vivants occuperaient une niche écologique qui leur est propre (sources de nourriture, prédateurs, lieux de reproduction, etc.). Cependant, lors d’un changement d’environnement, des organismes peuvent entrer en compétition l’un avec l’autre si leurs habitats ont été bouleversés. Par exemple, si une espèce se retrouve sur un nouveau territoire, celle-ci peut se retrouver en lutte avec l’organisme qui occupe la même niche écologique menant à un écartement de l’envahisseur ou du natif. Ceci est notamment le cas des espèces invasives en général (souvent observé chez les insectes) qui colonisent des territoires entiers. Un autre exemple bien connu est celui de l’écureuil gris américain qui a été introduit en Angleterre et XIXème siècle et qui a colonisé le pays en poussant l’écureuil roux vers la quasi extinction(16).
L’arrivée de l’épidémie du COVID-19 a perturbé la circulation de plusieurs virus respiratoires, souvent attribuée aux mesures sanitaires qui auraient influencé/écarté la circulation des autres virus(17), mais également au phénomène d’interférence virale (18). L’interférence virale a été décrite dans quelques publications avec fréquemment le rhinovirus (un des nombreux virus responsables du rhume) excluant les autres virus, dont le virus de la grippe (19), et plus spécifiquement celui responsable de l’épidémie de 2009, le H1N1 (20), les coronavirus en général(21)(22) et probablement le SARS-CoV‑2(23). Mais il existe naturellement moins de données entre la grippe et le SARS-CoV‑2…Les quelques observations à disposition concernent l’arrivée de la pandémie en début 2020, lorsque la grippe de la saison 2019–2020 était présente. Une publication qui étudie les co-infections grippe + coronavirus a également observé une diminution de 68% du risque de contracter le SARS-CoV‑2 si on était déjà infecté par la grippe(24). D’autres études observationnelles(25) et menées au laboratoire(26) ont également conclu que les coronavirus (dont le SARS-CoV‑2) et les virus de la grippe entretiennent une relation antagoniste.
Le SARS-CoV‑2 étant en compétition avec la grippe et ayant probablement été responsable de la disparition de cette dernière par interférence virale, la réapparition récente de la grippe en Belgique(27) (fin 2021-début 2022) serait donc plutôt une bonne nouvelle. Cela voudrait dire que les variants actuels du SARS-CoV‑2 ne présentent plus la même menace que les précédents, n’arrivant pas à écarter les virus de la grippe…Ce qui, à son tour, signifierait que la pandémie du COVID-19 serait terminée. Ceci rejoint également les observations sur la mortalité causée par les variants successifs, de moins en moins virulents(28). D’ailleurs, l’historien des sciences David Robertson et l’éditeur de la revue scientifique prestigieuse British Medical Journal, Peter Doshi, nous ont récemment rappelé que la fin des pandémies passées n’a pas été liée à la transmission des maladies ou leur pathogénicité, mais plutôt à des aspects sociologiques et plus précisément à l’attention que prête le grand public, les médias et les décideurs politiques à l’épidémie en cours(29). En effet, il s’agit de s’interroger sur les arguments qui permettraient de déclarer la fin d’une pandémie: la circulation du virus? La mortalité? Les variants successifs ont été de moins en moins létaux… Et le virus pourrait devenir endémique (naturel chez l’homme). Si c’est au grand public de se désintéresser de cette maladie, dont la menace perd de son importance tous le jours, il en revient donc à nous de décider de la fin de la pandémie…
Mais annoncer la fin de la pandémie aurait de fortes conséquences économiques sur les entreprises pharmaceutiques qui fournissent les vaccins. S’agrippant à la stratégie vaccinale, la société Moderna (dont les chiffres d’affaires avaient augmenté de 4708,44 % en 2021 comparé à 2020(30) a annoncé le 09 septembre 2021 qu’elle était en cours de développement d’un vaccin polyvalent combinant 6 ARNm différents(31) contre le COVID-19, la grippe et le virus respiratoire syncytial (RSV, un virus causant des bronchiolites dont la circulation a également été perturbée par le SARS-CoV‑2(32). De plus, Novavax a également initié le développement d’un double vaccin contre le SARS-CoV‑2 et la grippe(33). Il est aisément possible d’imaginer la promotion de ces vaccins par les autorités sanitaires. D’une part, appelant à éviter une future épidémie d’un variant hypothétique du SARS-CoV‑2 et d’autre part, à bénéficier simultanément d’une protection contre la grippe saisonnière et le RSV. Seulement, plusieurs problèmes dans l’efficacité de ces vaccins peuvent d’ores et déjà être soulevés:
- La mise à jour des vaccins contre la grippe saisonnière se base sur des souches virales circulant ailleurs sur la planète (constituant une des raisons de leur inefficacité), or la grippe a été absente pendant la pandémie. Même les vaccins administrés pour le COVID-19 se basent encore sur la souche originale « wuhan » malgré tous les variants qui ont émergé depuis le début de l’épidémie, ce qui témoigne de la difficulté des mises à jour
- Les vaccins à ARNm sont encore à un stade précoce de leur utilisation (et en phase d’étude(34)) et leurs effets secondaires toujours en cours de recensement
- La grippe peut causer des problèmes cardiaques(35), comme des myocardites(36), probablement liés à la nature des ses protéines de surface(37) (leur équivalent de la protéine « spike »). Rappelons que similairement à la grippe, la nocivité de la protéine spike du SARS-CoV‑2 a été démontrée et les effets secondaires des vaccins observés sont très probablement liés à celle-ci(38). Il n’est donc pas déraisonnable de se poser la question de la toxicité de nouveaux vaccins à ARNm s’ils se basent sur les protéines de surface de ces virus. La vaccination généralisée risquerait de provoquer des problèmes auprès des personnes qui ne sont pas à risque. Il convient dans ce contexte de rappeler les effets secondaires des vaccins contre la grippe H1N1, qui incluait la narcolepsie (pour le vaccin Pandemrix)(39). Ceci témoigne de l’importance cruciale d’effectuer des études cliniques robustes en prenant le temps nécessaire pour obtenir des vaccins efficaces et inoffensifs (autant que faire se peut) et d’administrer ces derniers à des personnes à risque.
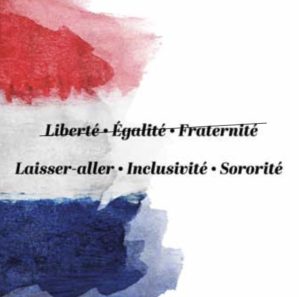
Agrippa est un nom d’origine romaine signifiant « naître les pieds en avant ». Dans l’Antiquité Romaine, ce type de naissance était considéré comme un signe funeste pour l’avenir. Annoncer une double épidémie à la fin d’une pandémie, qui serait celle du COVID-19 et la grippe (A?) me paraît être un signe bien funeste d’une volonté de maintenir les mesures sanitaires (y compris la vaccination), alors que toutes les données scientifiques indiquent qu’il est temps de siffler la fin de la pandémie.
- Quelques exemples d’articles de la presse internationale relayant la crainte d’une double épidémie grippe+corona: En Belgique: La Grippe risque de se mêler au coronavirus, cette année: les experts insistent sur la vaccination. RTL, 28 août 2020: https://www.rtl.be/info/magazine/sante/la-grippe-risque-de-se-meler-au-coronavirus-cette-annee-les-experts-insistent-sur-la-vaccination-1240356.aspx , En France: Coronavirus et grippe: l’inquiétude d’une double épidémie hivernale. Top Santé, 19 août 2020: https://www.topsante.com/medecine/troubles-orl/grippe/double-epidemie-hivernale-vaccin-grippe-638140 , Au Canada: Grippe et COVID-19: vers une épidémie double à l’automne? Québec Science, 27 août 2020: https://www.quebecscience.qc.ca/sciences/grippe-covid-19-epidemie-double-automne/
- Fearing a « twindemic » Health Experts Push Urgently for Flu Shots. New York Times, 16 août 2020: https://www.nytimes.com/2020/08/16/health/coronavirus-flu-vaccine-twindemic.htm
- Bulletin hebdomadaire infections respiratoires. Semaine / week 02 (10/01/2022–16/01/2022). Sciensano: https://www.sciensano.be/sites/default/files/influenza_2022_02.pdf , Seasonal influenza 2020−2021. Annual Epidemiological Report. Centre Européen de Prévention et de Contrôle des Maladies: https://www.ecdc.europa.eu/sites/default/files/documents/AER-seasonal-influenza-2020-final.pdf , Spantideas N, Bougea A M, Drosou E G, et al. (September 15, 2021) COVID-19 and Seasonal Influenza: No Room for Two. Cureus 13(9): e18007. doi:10.7759/cureus.18007 , Hagen, A., 2021. COVID-19 and the Flu. American Society for Microbiology.
- Return of the flu: EU faces threat of prolonged ‘twindemic’. Reuters, 17 janvier 2022: https://www.reuters.com/world/europe/return-flu-eu-faces-threat-prolonged-twindemic-2022–01-17/
- Influenza – estimating burden of disease. Organisation Mondial de la Santé: https://www.euro.who.int/en/health-topics/communicable-diseases/influenza/seasonal-influenza/burden-of-influenza
- Idem référence n°4
- COVID-19: People who catch coronavirus and flu at same time this winter ‘twice as likely to die’, Jenny Harries warns, amid fears of ‘twindemic’. Skynews, 10 octobre 2021: https://news.sky.com/story/covid-19-people-who-catch-coronavirus-and-flu-at-same-time-this-winter-twice-as-likely-to-die-jenny-harries-warns-12430502
- Idem référence n°4
- Idem référence N°1 et 4, ainsi que Devra-t-on se faire vacciner contre la grippe en même temps que contre le Covid? Le Parisien, 15 septembre 2021: https://www.leparisien.fr/societe/sante/devra-t-on-se-faire-vacciner-contre-la-grippe-en-meme-temps-que-contre-le-covid-15–09-2021-KRY36EXODFHH3PTPB3IG56ODXU.php
- Influenza vaccine effectiveness. Centre Européen de Prévention et de Contrôle des Maladies: https://www.ecdc.europa.eu/en/seasonal-influenza/prevention-and-control/vaccine-effectiveness
- Ad Doxa per Aspera: https://www.kairospresse.be/ad-doxa-per-aspera/
- Stowe J, Tessier E, Zhao H, Guy R, Muller-Pebody B, Zambon M, Andrews N, Ramsay M, Lopez Bernal J. Interactions between SARS-CoV‑2 and influenza, and the impact of coinfection on disease severity: a test-negative design. Int J Epidemiol. 2021 Aug 30;50(4):1124–1133. doi: 10.1093/ije/dyab081. PMID: 33942104; PMCID: PMC81357028 , Yue H, Zhang M, Xing L, Wang K, Rao X, Liu H, Tian J, Zhou P, Deng Y, Shang J. The epidemiology and clinical characteristics of co-infection of SARS-CoV‑2 and influenza viruses in patients during COVID-19 outbreak. J Med Virol. 2020 Nov;92(11):2870–2873. doi: 10.1002/jmv.26163. Epub 2020 Jul 6. PMID: 32530499; PMCID: PMC7307028.
- Kim D, Quinn J, Pinsky B, Shah NH, Brown I. Rates of Co-infection Between SARS-CoV‑2 and Other Respiratory Pathogens. JAMA. 2020 May 26;323(20):2085–2086. doi: 10.1001/jama.2020.6266. PMID: 32293646; PMCID: PMC7160748.
- Mandelia Y, Procop GW, Richter SS, Worley S, Liu W, Esper F. Dynamics and predisposition of respiratory viral co-infections in children and adults. Clin Microbiol Infect. 2021 Apr;27(4):631.e1-631.e6. doi: 10.1016/j.cmi.2020.05.042. Epub 2020 Jun 12. PMID: 32540470.
- Goka EA, Vallely PJ, Mutton KJ, Klapper PE. Single, dual and multiple respiratory virus infections and risk of hospitalization and mortality. Epidemiol Infect. 2015 Jan;143(1):37–47. doi: 10.1017/S0950268814000302. Epub 2014 Feb 24. PMID: 24568719. , Pinky L, Dobrovolny HM. Coinfections of the Respiratory Tract: Viral Competition for Resources. PLoS One. 2016;11(5):e0155589. Published 2016 May 19. doi:10.1371/journal.pone.0155589
- Science et Avenir. L’écureuil gris supplante le roux en Europe à cause… de l’homme. 16 janvier 2016: https://www.sciencesetavenir.fr/animaux/biodiversite/l‑ecureuil-gris-supplante-le-roux-en-europe-a-cause-de-l-homme_103513
- Groves HE, Piché-Renaud PP, Peci A, Farrar DS, Buckrell S, Bancej C, Sevenhuysen C, Campigotto A, Gubbay JB, Morris SK. The impact of the COVID-19 pandemic on influenza, respiratory syncytial virus, and other seasonal respiratory virus circulation in Canada: A population-based study. Lancet Reg Health Am. 2021 Sep;1:100015. doi: 10.1016/j.lana.2021.100015. Epub 2021 Jul 17. PMID: 34386788; PMCID: PMC8285668. , Oh DY, Buda S, Biere B, Reiche J, Schlosser F, Duwe S, Wedde M, von Kleist M, Mielke M, Wolff T, Dürrwald R. Trends in respiratory virus circulation following COVID-19-targeted nonpharmaceutical interventions in Germany, January — September 2020: Analysis of national surveillance data. Lancet Reg Health Eur. 2021 Jul;6:100112. doi: 10.1016/j.lanepe.2021.100112. Epub 2021 Jun 7. PMID: 34124707; PMCID: PMC8183189. , Olsen SJ, Winn AK, Budd AP, Prill MM, Steel J, Midgley CM, Kniss K, Burns E, Rowe T, Foust A, Jasso G, Merced-Morales A, Davis CT, Jang Y, Jones J, Daly P, Gubareva L, Barnes J, Kondor R, Sessions W, Smith C, Wentworth DE, Garg S, Havers FP, Fry AM, Hall AJ, Brammer L, Silk BJ. Changes in Influenza and Other Respiratory Virus Activity During the COVID-19 Pandemic — United States, 2020–2021. MMWR Morb Mortal Wkly Rep. 2021 Jul 23;70(29):1013–1019. doi: 10.15585/mmwr.mm7029a1. PMID: 34292924; PMCID: PMC8297694.
- Jones N. How COVID-19 is changing the cold and flu season. Nature. 2020 Dec;588(7838):388–390. doi: 10.1038/d41586-020–03519‑3. PMID: 33324005. , Sarvepalli SS, Cruz ABV, Chopra T, Salimnia H, Chandrasekar P. Striking absence of “usual suspects” during the winter of the COVID-19 pandemic. Presenté au: European Congress of Clinical Microbiology & Infectious Diseases; July 9–12, 2021. Abstract 02678. Accessed July 9, 2021. https://drive.google.com/file/d/1yqjPOsxTG5fOcmf1WSABvlRtPn2fcMo_/view
- Nickbakhsh S, Mair C, Matthews L, Reeve R, Johnson PCD, Thorburn F, von Wissmann B, Reynolds A, McMenamin J, Gunson RN, Murcia PR. Virus-virus interactions impact the population dynamics of influenza and the common cold. Proc Natl Acad Sci U S A. 2019 Dec 16;116(52):27142–50. doi: 10.1073/pnas.1911083116. Epub ahead of print. PMID: 31843887; PMCID: PMC6936719.
- Wu A, Mihaylova VT, Landry ML, Foxman EF. Interference between rhinovirus and influenza A virus: a clinical data analysis and experimental infection study. Lancet Microbe. 2020 Oct;1(6):e254-e262. doi: 10.1016/s2666-5247(20)30114–2. Epub 2020 Sep 5. PMID: 33103132; PMCID: PMC7580833.
- Idem référence n°18
- Grimwood K, Lambert SB, Ware RS. Endemic Non-SARS-CoV‑2 Human Coronaviruses in a Community-Based Australian Birth Cohort. Pediatrics. 2020 Nov;146(5):e2020009316. doi: 10.1542/peds.2020–009316. Epub 2020 Sep 4. PMID: 32887791.
- Idem référence n°19 , Kiseleva I, Ksenafontov A. COVID-19 Shuts Doors to Flu but Keeps Them Open to Rhinoviruses. Biology (Basel). 2021 Jul 31;10(8):733. doi: 10.3390/biology10080733. PMID: 34439965; PMCID: PMC8389621.
- Stowe J, Tessier E, Zhao H, Guy R, Muller-Pebody B, Zambon M, Andrews N, Ramsay M, Lopez Bernal J. Interactions between SARS-CoV‑2 and influenza, and the impact of coinfection on disease severity: a test-negative design. Int J Epidemiol. 2021 Aug 30;50(4):1124–1133. doi: 10.1093/ije/dyab081. PMID: 33942104; PMCID: PMC8135706.
- Spantideas N, Bougea AM, Drosou EG, Khanderia N, Rai S. COVID-19 and Seasonal Influenza: No Room for Two. Cureus. 2021 Sep 15;13(9):e18007. doi: 10.7759/cureus.18007. PMID: 34667682; PMCID: PMC8516323.
- Halfmann PJ, Nakajima N, Sato Y, Takahashi K, Accola M, Chiba S, Fan S, Neumann G, Rehrauer W, Suzuki T, Kawaoka Y. SARS-CoV‑2 Interference of Influenza Virus Replication in Syrian Hamsters. J Infect Dis. 2022 Jan 18;225(2):282–286. doi: 10.1093/infdis/jiab587. PMID: 34875072; PMCID: PMC8689717. , Peng JY, Shin DL, Li G, Wu NH, Herrler G. Time-dependent viral interference between influenza virus and coronavirus in the infection of differentiated porcine airway epithelial cells. Virulence. 2021 Dec;12(1):1111–1121. doi: 10.1080/21505594.2021.1911148. PMID: 34034617; PMCID: PMC8162253.
- Idem référence n°3
- Données consultables par exemple sur le site Our World in Data ou John Hoptkins Coronavirus Resource Center
- Robertson D, Doshi P. The end of the pandemic will not be televised. BMJ. 2021 Dec 14;375:e068094. doi: 10.1136/bmj-2021–068094. PMID: 34906970.
- https://www.macrotrends.net/stocks/charts/MRNA/moderna/revenue
- https://investors.modernatx.com/news/news-details/2021/Moderna-Announces-Significant-Advances-Across-Industry-Leading-mRNA-Portfolio-at-2021-RD-Day-09–09-2021/default.aspx , https://twitter.com/moderna_tx/status/1435978825377136641?lang=fr , https://www.reuters.com/business/healthcare-pharmaceuticals/moderna-developing-single-dose-combination-vaccine-covid-19-flu-2021–09-09/
- Di Mattia G, Nenna R, Mancino E, Rizzo V, Pierangeli A, Villani A, Midulla F. During the COVID-19 pandemic where has respiratory syncytial virus gone? Pediatr Pulmonol. 2021 Oct;56(10):3106–3109. doi: 10.1002/ppul.25582. Epub 2021 Jul 26. PMID: 34273135; PMCID: PMC8441855.
- https://www.reuters.com/business/healthcare-pharmaceuticals/novavax-begins-early-stage-trial-combined-influenzacovid-19-vaccine-2021–09-08/
- Exemple pour Pfizer BioNTech: https://clinicaltrials.gov/ct2/show/NCT04368728
- Estabragh ZR, Mamas MA. The cardiovascular manifestations of influenza: a systematic review. Int J Cardiol. 2013 Sep 10;167(6):2397–403. doi: 10.1016/j.ijcard.2013.01.274. Epub 2013 Mar 7. PMID: 23474244.
- Baral N, Adhikari P, Adhikari G, Karki S. Influenza Myocarditis: A Literature Review. Cureus. 2020 Dec 10;12(12):e12007. doi: 10.7759/cureus.12007. PMID: 33437555; PMCID: PMC7793451.
- Seeherman S, Suzuki YJ. Viral Infection and Cardiovascular Disease: Implications for the Molecular Basis of COVID-19 Pathogenesis. Int J Mol Sci. 2021 Feb 7;22(4):1659. doi: 10.3390/ijms22041659. PMID: 33562193; PMCID: PMC7914972.
- Détaillés par Kaarle Parikka dans le livret: COVID-19 Par delà la censure. Collectif Elaia. Édition : GRAPPE Réf. ISBN : 9782960288308
- Sarkanen T, Alakuijala A, Julkunen I, Partinen M. Narcolepsy Associated with Pandemrix Vaccine. Curr Neurol Neurosci Rep. 2018 Jun 1;18(7):43. doi: 10.1007/s11910-018‑0851‑5. PMID: 29855798.